Why “Nothing Is Wrong” Still Feels So Wrong
Feeling off but nothing is wrong?
There’s a particular kind of frustration that comes from being told you’re fine—when something in you keeps whispering, something is wrong.
You go to the doctor. You do the physical examination. You do the labs. Maybe you get imaging. You answer the same questions about other symptoms again and again. The results come back “normal,” and you’re told you’re in good shape—your overall health looks fine.
And yet, in your daily life, you don’t feel fine.
Not in a dramatic, headline way. More in the quiet way that changes how you move through the day: you’re feeling tired earlier than you used to, your energy levels don’t rebound, your focus is harder to hold, your to do list feels heavier than it should, and you can’t quite get traction. You might feel overwhelmed by decisions that used to be simple. You might notice negative feelings that don’t match your circumstances. You might feel a low-grade “blah” that’s hard to explain—almost like experiencing malaise, a sense of overall weakness that lingers.
That “in-between” state is common. It’s also easy to dismiss—especially when the outside world keeps telling you you’re okay.
This post is here to name what that experience often means, why it matters, and what kind of support helps—without turning your life into another stress management project.
When “Normal” Results Don’t Match Your Lived Experience
Modern medicine is excellent at identifying urgent, measurable problems. If you have bacterial infections, many medical conditions, or clearly defined patterns that show up on tests, there are often straightforward next steps. That’s a good thing.
But “normal results” usually means: nothing obvious has crossed a diagnostic threshold. It does not necessarily mean there isn’t an underlying cause to how you feel.
This is where many people get stuck.
You might be told to look at lifestyle factors: improve your healthy diet, get enough sleep, cut back on alcohol, add regular exercise, and focus on managing stress. Those are all valid foundations. They can support well being and emotional health. They can absolutely improve symptoms for some people.
But sometimes the experience persists even when you’re doing the “right” things.
Sometimes you’re already the person who tries hard:
you take care of your mental state
you keep responsibilities moving
you stay functional for work and family
you keep a social life (or at least try)
you do the “healthy habits” and still feel exhausted
And when that happens, the gap between what you’re told and what you experience can start to mess with your confidence. It can quietly impact self esteem. It can make you question your perception: “Am I making this up? Is it just anxiety? Is it depression? Is this a mental illness thing?”
Some people get referred to talk therapy or clinical psychology. For many, that’s supportive—especially if you’re dealing with grief, trauma, relationship stress, or mental health issues. Talk therapy can help you understand patterns, make meaning, and feel less alone. A support group can also be a lifeline when you’re carrying a lot.
But here’s the important nuance: even when talk helps, it may not fully resolve the body-level strain underneath it.
And sometimes, receiving a label can create its own confusion. You might read about mental disorders or the Diagnostic and Statistical Manual, and wonder whether you “fit.” You might worry you’re developing something serious. You might fear you’re missing a diagnosis. Or you might feel relieved to have a name—yet still sense that the name doesn’t fully explain the felt experience in your body.
If this is you, you’re not broken. You’re not behind. You’re not failing at self-care.
There is often a missing layer in the conversation.
The Missing Piece: Load That Doesn’t Show Up on Tests
There are forms of strain that don’t always register in a blood panel or a single office visit. They show up in patterns—in how your system holds tension, how quickly you get depleted, how hard it is to return to the present moment, and how long it takes to recover after stressful situations.
This is especially common when you’ve been living with:
ongoing stress that never fully resolves
chronic responsibilities or too many responsibilities
big lifestyle changes (a move, divorce, empty nesting, caregiving, grief, health shifts)
sleep disruption (including sleep apnea, or fragmented sleep that looks like “enough” hours but doesn’t restore)
long periods of pushing through because you had no other option
Sleep deprivation, even one poor night, can weaken the brain's ability to regulate emotions. High-speed digital lives can prevent the brain from engaging in self-reflection and emotional processing. Unresolved trauma can affect mood and emotional responses later in life. Hormonal changes can lead to emotional instability. People also often feel stuck in their lives when they perceive that others have things figured out while they do not.
When this load accumulates, your body gets good at compensation. It adapts. It becomes efficient. It learns to keep going even when resources are low. From the outside, you can look “fine.” Inside, your baseline may be strained.
Over time, this can look like:
needing more downtime than you used to, but not being able to truly rest
being more sensitive to noise, light, or interruption
feeling “keyed up” at night and slow in the morning
feeling emotionally flat, quick to irritability, or stuck in negative feelings
being social, then crashing afterward
a sense of “I can’t catch up,” even when nothing is actively wrong
Many people respond by trying harder. They optimize their routine. They take on more tools. They become more disciplined. But if the strain is cumulative, that can backfire—because it turns recovery into a job.
Why Trying Harder Usually Makes It Worse
When you don’t feel well and no clear diagnosis appears, it’s natural to start troubleshooting. You look for common causes. You change your healthy diet. You increase regular exercise. You try to improve sleep. You cut back on alcohol. You search for the perfect supplement stack. You add meditation apps, journaling prompts, and more structure.
And to be clear: some of these help. Many people need exactly those foundations.
But if your system has been compensating for a long time, “more effort” can become just another demand.
This is where people say:
“I’m doing all the stress management things and I still feel overwhelmed.”
“I’m getting enough sleep and I still feel tired.”
“I’m doing therapy and I understand why I feel this way… but I still don’t feel better.”
“My body feels like it’s always bracing.”
Sometimes you try techniques like deep breathing or progressive muscle relaxation. Those can be helpful, especially in the moment. They can reduce intensity. They can steady you during an anxious spike.
Chronic stress increases cortisol, which disrupts mood-regulating brain chemicals like serotonin and dopamine. Burnout is a gradual process that doesn't happen overnight, but can creep up on you. The signs and symptoms of burnout are subtle at first, but become worse as time goes on.
But if you’re using them to override your signals rather than process what’s underneath, they can become another form of control—another way of saying, “Not now. Keep it together.”
And when your life is already full—when your calendar is packed, your bandwidth is thin, and your to do list is relentless—regulation becomes one more task you have to complete correctly.
That’s exhausting.
When Coping Becomes Another Job
This is the part people rarely say out loud: sometimes the tools that are supposed to help you feel better become part of the strain.
You might notice:
you “should” meditate, but it feels like work
you “should” do breathwork, but it becomes performance
you “should” be more positive, but positivity feels like pressure
you “should” be grateful, but gratitude doesn’t restore energy
If you’ve ever had a panic attack (or something close to it), you may have learned to manage symptoms quickly—breathing, grounding, distraction. Useful skills. But many people discover later that managing symptoms isn’t the same as resolving the load that made the system tip in the first place.
Over time, constant managing can quietly erode trust in your body. You become hyper-aware of your internal state, scanning for signs you’re not okay. You may feel anxious about your anxiety. You may feel depressed about your lack of motivation. You may worry your mental health issues are worsening—even when what’s really happening is exhaustion plus long-term strain.
This is why people can end up in a loop: searching for the right tool to fix what feels off, while the underlying load continues.
What Your Body Is Actually Asking For
When you feel off but nothing is “wrong” on paper, your body is often asking for something different than more strategies.
It’s asking for conditions where it can:
settle enough to stop bracing
complete stress responses that got interrupted
restore rhythm and internal pacing
rebuild capacity—so the same life feels less effortful
This is not about willpower. It’s not about doing awareness “better.” It’s about giving your system enough safety and space to do what it couldn’t fully do while it was busy keeping you functional.
If you’ve lived with chronic strain, the goal isn’t a single “fix.” It’s a return of options.
Options like:
being present without forcing it
having energy after work, not only before
feeling connected in your social life without paying for it later
experiencing emotions without being flooded by them
making decisions without feeling like every choice costs too much
These are the quiet markers of real resilience.
Why One-Time Relief Isn’t Enough for Some Systems
A lot of people are fine with occasional resets. A massage. A weekend off. A good night of sleep. A vacation. A short burst of therapy. A few weeks of healthier eating.
But for many people—especially those with chronic responsibilities, chronic symptoms, or long-term adaptation—relief tends to come through return.
Return to downshifting.
Return to safety.
Return to internal pacing.
Return to a baseline that feels coherent.
This is why some people feel better after a supportive session, then realize the deeper benefit comes from consistency. Not because something is wrong with them, but because their system has been carrying load for a long time. It takes time to unwind compensation.
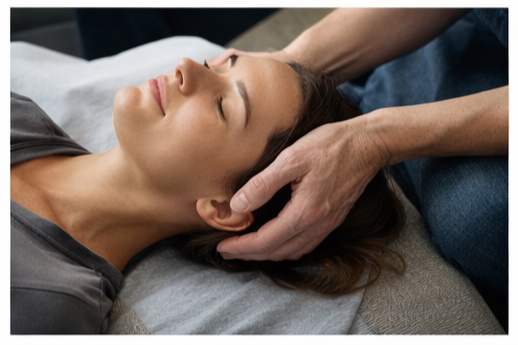
Why Body-Based Support Can Feel Different
This is where approaches like Craniosacral Therapy and other forms of somatic therapy can be meaningful. They work with the body’s patterns of holding and adaptation—patterns that don’t always shift through insight alone.
Talk therapy can be profoundly supportive. It can help you make sense of your story, improve relationships, strengthen boundaries, and bring clarity to your life. It can support self-worth. It can help you name what you’ve been carrying.
Body-based work addresses a different layer: the physiological patterns that persist even after you understand the “why.”
Instead of asking you to think your way into calm, it supports the system’s ability to settle from the inside out—so your baseline has a chance to change.
And “gentle” doesn’t mean shallow. Gentle input can be exactly what allows deeper patterns to soften, because the body doesn’t have to defend itself against force.
Gentle Doesn’t Mean Passive
For many sensitive, high-functioning people, force is familiar: push through, stay strong, keep going, make it work. Even self-care can become forceful when it’s approached like a performance.
Body-based work is different. It’s often slower. It’s more receptive. It’s built around listening rather than striving.
For some people, that’s uncomfortable at first—because it asks you to stop managing. It asks you to notice. It asks you to allow your system to reorganize in its own timing.
But when that shift happens, people often describe changes that are hard to quantify yet very real:
less bracing in the body
more stable energy
clearer focus
fewer spikes of overwhelm
improved ability to stay in the present moment
Not because life becomes easy, but because your baseline becomes more resilient.
Feeling Like Yourself Again Is a Process, Not a Switch
Most people want a clear answer: “What’s the diagnosis?” “What’s the treatment?” “What’s the plan?”
But when you’re in this in-between space, the path is often more like a gradual return than a dramatic turnaround.
You may start noticing:
your energy doesn’t crash as hard
you can handle stressful situations with less aftermath
your sleep becomes more restorative (even if it’s not perfect)
you can feel emotions without being taken over by them
your sense of well being returns in small, steady ways
These are not flashy changes. They’re the kind that quietly improve everything—work, relationships, decision-making, health habits, and your capacity to enjoy your life.
If Something in You Knows This Isn’t Nothing
If you recognize yourself in this—not just intellectually, but viscerally—that matters.
Many people wait until they have clear, measurable specific symptoms before they allow themselves support. Others wait for a crisis. Some wait until they’ve tried every tool. Some wait because they fear being told it’s “just anxiety” or “just depression.” Some worry they’re headed toward something serious—toward a diagnosis, toward a label, toward “real” illness.
But the truth is: you don’t need to prove you’re struggling in order to deserve support.
If you’re repeatedly asking, “Why do I feel this way?”
If your body keeps signaling that something is off—despite normal tests—
If you feel like you’re functioning, but paying for it constantly—
…that is information.
And responding to that information early can change the trajectory of your health over time.
What This Middle Space Is Pointing Toward
If you’ve been told “nothing is wrong,” but you don’t feel okay, trust your lived experience.
This isn’t about catastrophizing. It’s about listening.
Sometimes the path forward is straightforward: you find a medical explanation, address a clear underlying issue, treat sleep apnea, correct deficiencies, adjust medication, recover from infection, or make practical lifestyle changes. Sometimes a healthcare provider finds what was missed the first time. Sometimes there is a medical condition that needs direct treatment.
And sometimes, the deeper need is support at the level of regulation and recovery—support that helps your body stop compensating so intensely.
The cost of ignoring this middle space is rarely immediate. It’s cumulative. Over time, life can get smaller. You may do less not because you don’t want to, but because you don’t have the reserves. Your social life may shrink. Your confidence may erode. Your joy may feel harder to access. You may start to believe you’re “just like this now.”
But you don’t have to accept that as your new normal.
There are kinds of support designed specifically for this layer—when you’re not in crisis, but you’re not at ease.
🗒️ A quick note about “mental” versus “physical”
It can be unsettling when the only explanations offered are “stress” or “anxiety,” as if your symptoms are purely psychological. In reality, your emotional health and your physiology aren’t separate systems competing for truth. They’re intertwined. What you think, what you feel, and what your body is carrying all influence your mental state—and vice versa.
That’s why the most helpful care is often layered. For some people, talk therapy is essential. For others, lifestyle changes make a noticeable difference. For others, somatic therapy is the missing piece that helps the body finally stand down. And for many people, it’s a combination over time—guided by what actually helps you function and feel like yourself again, not by what looks best on paper.
This is the kind of work held experientially inside the Observatory.
Not by giving you more to manage, but by creating the conditions for your body to restore balance.